Anonymous
Some time last year, I went to the sexual health clinic with the usual symptoms of vaginal thrush – a change in discharge, itching and discomfort. I was seen by a doctor, examined and given the suitable medication for what was, indeed, thrush. My vulva soon returned to its normal state, and I continued my life as usual.
A few months later, I again started to experience what I believed to be the symptoms of vaginal thrush. I had a quick google and reluctantly decided that I should probably go to the sexual health clinic, again (admittedly mainly because they give you the medication and cream for free). I waited the usual hour at the drop-in and was examined by a nurse. When she inserted the speculum I cried out because it hurt and held back the tears that pricked my eyes. She said that she couldn’t see any symptoms of thrush and that, this time round, it was actually my cervix that looked red and inflamed. The nurse told me that I shouldn’t have sex until the pain had reduced, and that the discharge was probably something to do with my inflamed cervix. I left the clinic feeling confused and still experiencing pain and discomfort.
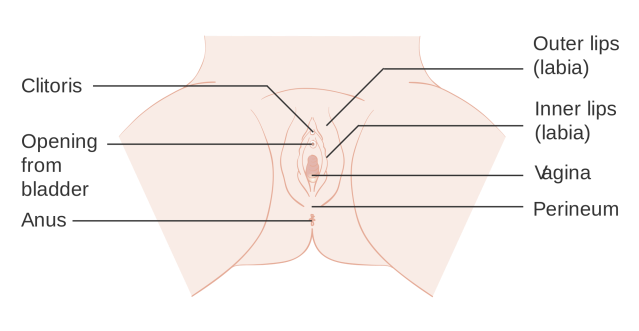
My symptoms of discomfort and burning did not go away, despite abstaining from sex. After a while, I decided that I would, again, return to the sexual health clinic. I waited the hour once more, and this time was seen by a doctor. I explained my symptoms and told her that I still thought it could be thrush and that I was worried about the pain I had been in for the last few months. The doctor was very understanding and decided she needed to examine me. I endured the pain of the speculum once more and was again told that my cervix was inflamed. When I told her that I only really experienced pain internally during sex, and that what I was concerned about was the pain around the entrance to my vagina, she said there was no obvious inflammation of my labia. I was reassured by her that the redness of my cervix was not a serious issue and sent away.
I performed this dance at my local sexual health clinic three more times over the next four to five months, one of the (male) nurses I saw during this time even had the audacity to say, “You know sometimes sex can hurt when you are not in love.” I even went to the sexual health clinic attached to my local hospital, where I was examined by a consultant, with no result.
I eventually broke down in hysterical tears to a nurse about the pain I was in. He looked at me, wide-eyed and unsure of what to do as I wailed “Nobody will help me,” and sobbed uncontrollably. He eventually went to get another woman nurse, who seemed irritated at his lack of resourcefulness, and offered to examine me. She said that I had been rubbing the painful area of my labia so much that it was red and raw and gave me some soothing cream and aqueous cream to wash with. It was only at this point that they finally referred me to the specialist psychosexual unit at the local hospital. Living with pain everyday had become normalised during all the months it took for me to finally get this referral.
After more than six months of sexual health drop-in clinics and GP appointments, I arrived at the hospital for my appointment with both a consultant and a psychologist. I was quizzed about every part of my sex life, my mental health and lifestyle. Deep down, I was uncomfortable at detailing intimate elements of my sex life to two strange middle-aged men, mentally flinching when they asked me how often I masturbate, but I performed my role as practical, open and relaxed patient, eager to get my appointment over and done with. Both doctors were very nice, but I was never given the option of seeing a woman consultant or being examined by a woman – the best they can offer you is a woman chaperone.
After the grilling and a further vaginal examination, the consultant diagnosed me with unprovoked vulvodynia. He assured me that I had done well to seek out medical support as quickly as I had, as many women endure the pain of vulvodynia for years before going to see their GP. He also informed me that lots of women report symptoms of vulvodynia after experiencing a couple of serious bouts of thrush, which I had never heard anyone talk about before. They gently started to explain the various treatments available, from medication to therapy, and I tried hard to conceal the fact that they had just smacked me in the face with a bag of bricks.
Vulvodynia is persistent, unexplained pain in the vulva which can be long-term and chronic, but the doctors assured me that much can be done to relieve the pain. It is not an STI, it is not infectious, it is not related to cancer and you cannot pass it on to a partner. In my case, unprovoked vulvodynia means that my pain is burning, sore and spontaneous in nature – it is not touching that causes the pain, it is there all the time.
I told them I was grateful that I had a diagnosis, but really, I felt worse being diagnosed with a long-term chronic pain issue than I had when I assumed the doctors were just missing some kind of skin condition. The doctor prescribed me medication that, in higher doses, is prescribed for depression. The reason for this being that the medication alters the way in which nerve fibres send their impulses to the spinal cord and give the sensation of pain. I remembered that there was once an episode of Sex & the City where Charlotte is diagnosed with vulvodynia and told she is going to be prescribed a “Light anti-depressant…for [her] vagina.” I want to smack whoever wrote this episode of Sex & the City into oblivion.
I left the consultant’s office, feeling numb, to go and pick up my medication from the hospital pharmacy. I cried quietly on a squeaky plastic chair in the waiting room and then got on the bus home. I felt stupid for crying and pulled myself together for the phone call to my partner. I explained that I had been prescribed this medication and that, hopefully, in a few weeks time, it would start to work and the pain I was in would be reduced.
Obviously when I got home the first thing I did was to google both Vulvodynia and the medication I had been prescribed. I found the encouraging news that the drug I am now on (amitriptyline) is effective for pain relief in 1/4 people, which is apparently very high…let’s hope I’m in that 25%. I also scrolled through various websites about amitriptyline where the warning DO NOT DRINK ALCOHOL as dangerous side effects or death can occur, was a consistent piece of advice. Amitriptyline also makes you drowsy, and I’ve been waking up in the mornings with a feeling similar to a hangover.
I am only in the first week of taking this medication and I know that it will take some time for doctors and/or psychologists to help me deal with the pain, but I cannot get over the amount of doctors visits it took for me to get the referral in the first place and that this actually only came after I sobbed hysterically to a bewildered nurse. GUM clinics are so stretched and understaffed that there was rarely a doctor there who was able to see me. This resulted in a cycle of being seen and made to leave with no diagnosis and no pain relief (ibuprofen and paracetamol do not work to relieve the pain of vulvodynia).
There is also the effect that this ordeal of almost a year has had on my mental health and sexual confidence. I have developed a level of anxiety around penetrative sex that I never had before, and sometimes it is too uncomfortable to have myself or another person even touching my vulva. I also never imagined that I would have had so many strange men examining and peering at my vulva, and how unpleasant I would find that experience.
I am hopeful that I will be able to take steps to relieve the pain that I’m experiencing over the next few months, but if I had been fully aware of what vulvodynia actually was, perhaps I would have been able to go to doctor with the vocabulary to explain my symptoms and have the confidence to ask for the help I needed. From my experience, there can be a distinct silence when it comes to the treatment of women’s sexual health. The difficulty, though, was that my inflamed cervix (which doctors did notice) had nothing to do with the vulvodynia. I believe this issue may have confused how I described my symptoms to doctors, but even so, it should have been picked up on that I was in physical pain with no external symptoms, given that I sought out medical help roughly ten times for the same issue.
I am ultimately thankful that I now know what is going on with my vulva and hope that my experience may help the up to 15% of women who have vulvodynia, and that it could also be a useful tool for those who will most probably never have heard of vulvodynia before. I found this website useful and have also discovered that there are vulvodynia groups on Facebook, including one for partners of women with vulvodynia.
My vulvodynia journey stretches on…hopefully it won’t continue to be this painful.

What an experience. It’s awful that so many visits to the clinic didn’t result in someone researching it further instead of sending you home with no diagnosis. I hope that treatment will be helpful for you.
Would you be comfortable if I shared this on my blog in case other women may learn from this blog post?
LikeLiked by 1 person
Yes that’s completely fine! Fingers crossed it all works out – I went to see another consultant yesterday and they confirmed the diagnosis so hopefully it will start to get better. Thanks for your comment
LikeLike
Three words: PELVIC FLOOR PHYSIOTHERAPY. I’ve had V for 7 years and it’s the one thing that’s made a colossal difference!
LikeLike
Thanks will look into it!
LikeLiked by 1 person
Thanks so much for writing this article. I’m so sorry you’ve been through this. I’ve had such a similar version of events to you it’s scary.
My journey started about 4 years ago and I just wanted to offer some hope! I’ve managed to get it under control multiple times and it’s actually only ever been really bad for 3 or so 4 month periods over the last 4 years. The rest of the time it was virtually no existent. I’m in a bad phase now, and terrified that it won’t get better so I understand how scary it is.
What started with thrush, I was eventually after seeing probably upwards of 20+ doctors and dozens of Sexual health checks I was diagnosed with unprovoked vulvodynia. Mine seems quite similar to you, like a burning / pain/ irritation and I often find it hard to believe it is vulvodynia as it seems so related to discharge etc.
I would love to chat to you more if you are keen – I don’t know anyone else with the condition and it would be awesome to share stories / treatment options.
Thanks
Harriet
LikeLike
Sorry it took me so long to reply to this Harriet (I’ve had such a hectic week!) I would love to chat to you more let’s get in contact via Facebook (I saw your comment on the Wolf Whistled page so will message you via there) It’s so great to hear from somebody in a similar position. Speak soon! XXX
LikeLike